Managing third-parties (insurers) you bill to
Before you bill a third-party for a service, you can enter the third-party into Wolf EMR as an insurer. If you don’t add a third-party as an insurer, you will have to enter the third-party’s contact information when you create a bill for the third-party. Also, when you add an insurer you can specify:
Whether the insurer’s invoices are to be sent via fax or mail
Whether ICD9 diagnostic codes can be included on bills for the insurer
Notes on how to invoice the insurer
How many days following a service the insurer can still be billed
What fee schedule is to be used for the insurer
What department or individual to address invoices to
Steps
| 1. | From the Wolf EMR home page, click Configuration |
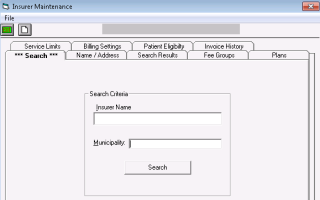
| 2. | From the Configuration menu, click View > Insurers, Payors (Gov’t, Private) and Codes > Insurers, Payors. The Insurer Maintenance window opens, with the Search tab selected. |
| 3. | Perform one of the following actions: |
To modify an insurer, search for an select the insurer:
| a) | In the Insurer Name field, enter all or part of the insurer’s name. |
| b) | In the Municipality field, enter the insurer’s municipality. |
Tip: To view a complete list of all insurers you bill to, leave the Insurer Name and Municipality fields blank.
| c) | Click Search. The EMR displays a list of matching insurers. |
| d) | In the list of insurers, click the insurer. |
The EMR displays the insurer Name / Address tab.
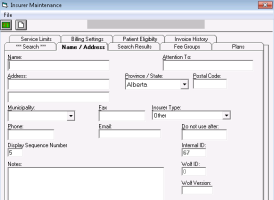
| 4. | In the Name / Address tab, enter or modify the insurer’s information using the following table as a reference. |
You can ignore fields that are not described in the following table.
| Field | Description |
|---|---|
|
Name |
Enter the name of the insurer, such as “ABC Law practice” or “ABC Insurance”. |
|
Attention To |
Enter the name of a contact person or department for invoices to be addressed to. Displays on invoices. |
|
Address fields |
Enter the insurer’s address. Displays on labels and invoices. |
|
Fax |
If you fax invoices to this insurer, the fax number entered here is used by default. |
|
Insurer Type |
In the list, select one of the following options: Patient: If bills are to be charged to the patient. Other: If bills are to be charged to a third party. The Patient option is typically used for only the generic Patient insurer. However, if you want patient bills to be grouped in your system based on services provided, you can create multiple patient insurers. For example, if you are a multi-disciplinary clinic, you can create a “Physiotherapy patient” insurer and a “Chiropractic patients” insurer. Your selection determines invoice format and fields displayed when billing. |
|
Phone |
Enter for your reference. |
|
Display Sequence Number |
Enter a number to specify how high on the Insurer list in the Billing window the insurer should display. (The Display Sequence Number determines sort order) The lower the number, the higher on the list the insurer displays. |
|
Notes |
Enter any notes regarding the insurer. For example, “Call for approval before sending invoice”. |
| 5. | To print address labels from the File menu, choose Print Address Label. You are prompted for the number to print. |
| 6. | Click Save |
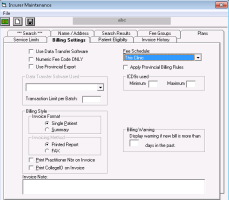
| 7. | Click the Billing Settings tab, and then enter billing details for the insurer using the following table as a reference. |
You can ignore fields that are not described in the following table.
| Field | Description |
|---|---|
|
Billing Style Invoicing Method |
Select if bills are to be printed/mailed, or faxed Printed Report: An individual Invoice is printed for each bill. Fax: An invoice is faxed to the fax number entered in the Name/Address tab. If there is no fax number entered in the Name/Address tab for the insurer, Fax is not available as an option. |
|
Print Practitioner Nbr on Invoice |
Select this check box to display the provider’s Prac ID on invoices created for the insurer. |
|
Fee Schedule |
In the list, select the fee schedule containing the fee codes you bill to the insurer. The most common selection is This Clinic. You can create a unique Fee Schedule (list of fees) for an insurer. See Creating fee schedules (fee lists). |
|
ICD9s used |
Enter the Minimum and Maximum number of ICD9 diagnostic codes you can add to bills for this insurer. For example, if you want to be able to enter up to three diagnostic codes on a bill, but not be required to enter a diagnostic code, enter 0 in the Minimum field, and then enter 3 in the Maximum field. The largest number of diagnosis codes you can enable is 3. This area is available only if, in the Fee Schedule list, you select a fee schedule that has ICD9 diagnostic codes enabled. |
|
Billing Warning |
Enter the number of days past the service date before you receive a warning from the EMR when you bill the insurer. If you create a bill to the insurer for a service provided more than the entered number of days in the past, a warning is generated before the bill is saved. For example, if the insurer requires that clinics add a note to a bill if the service date is 90 days or older, you would enter 90 in the Bill Warning area. If the service date is 90 days or older, billers receive the warning to add a note to the bill. |
|
Invoice Note |
Enter any notes or instructions on how to invoice the insurer. This information is for your reference only. |
| 8. | At the top of the window, click Save |
© 2018